Join our mailing list to receive the latest health tips and updates.
You have Successfully Subscribed!
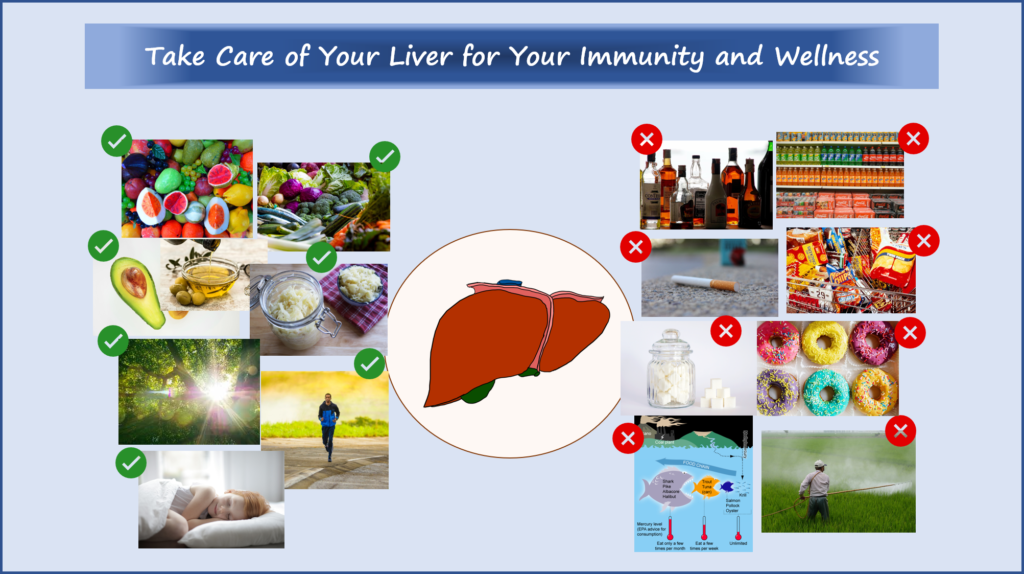
Take Care of Your Liver for Healthy Immunity and Overall Wellness
Liver is the largest internal organ in our body.
Liver conducts many critical biological functions including frontline immune defense against infections and protecting our body from toxins and other harmful substances.
Impaired liver function has widespread effects on our overall health and wellbeing.
Chronic liver disease may be more prevalent than one might think. More than 30% of US population are estimated to have chronic liver disease.1
Therefore, it is important to support liver health as part of our strategies for healthy immunity and overall wellness.
In this article, I share evidence-based information on liver functions in immune defense, risk factors that can promote liver dysfunction and diseases, and tips to support liver health..
For a quick summary of the tips to support liver health, you can go directly to the Summary section.
Topic List
Risk Factors for Liver Dysfunction and Diseases
Metabolic Disorders/Diseases (Obesity, Diabetes, Hypertension, Heart Disease)
Gut and Gut Microbiota Dysfunction
Industrial Fructose Consumption
Drug-Induced Liver Injury (DILI)
Dietary Choices to Support Liver Health
Lifestyle Choices to Support Liver Health
Specific Nutrients and Nutritional Compounds That Support Liver Health
Summary
Liver is a hard-working organ carrying out more than 500 vital biological functions as described in section Overview of Liver Functions.
Liver plays important roles in frontline immune defense against infections (see section Liver and Immunity).
Because of the its many vital functions, liver dysfunction and diseases often lead to many other chronic health conditions and diseases.
There are different types of liver disease as described in section Types of Liver Disease, where some are more common than others and increasingly become a global health concern.
Risk factors that promote the more common liver dysfunction and diseases are often related to diet and lifestyle choices (see section Risk Factors for Liver Dysfunction and Diseases).
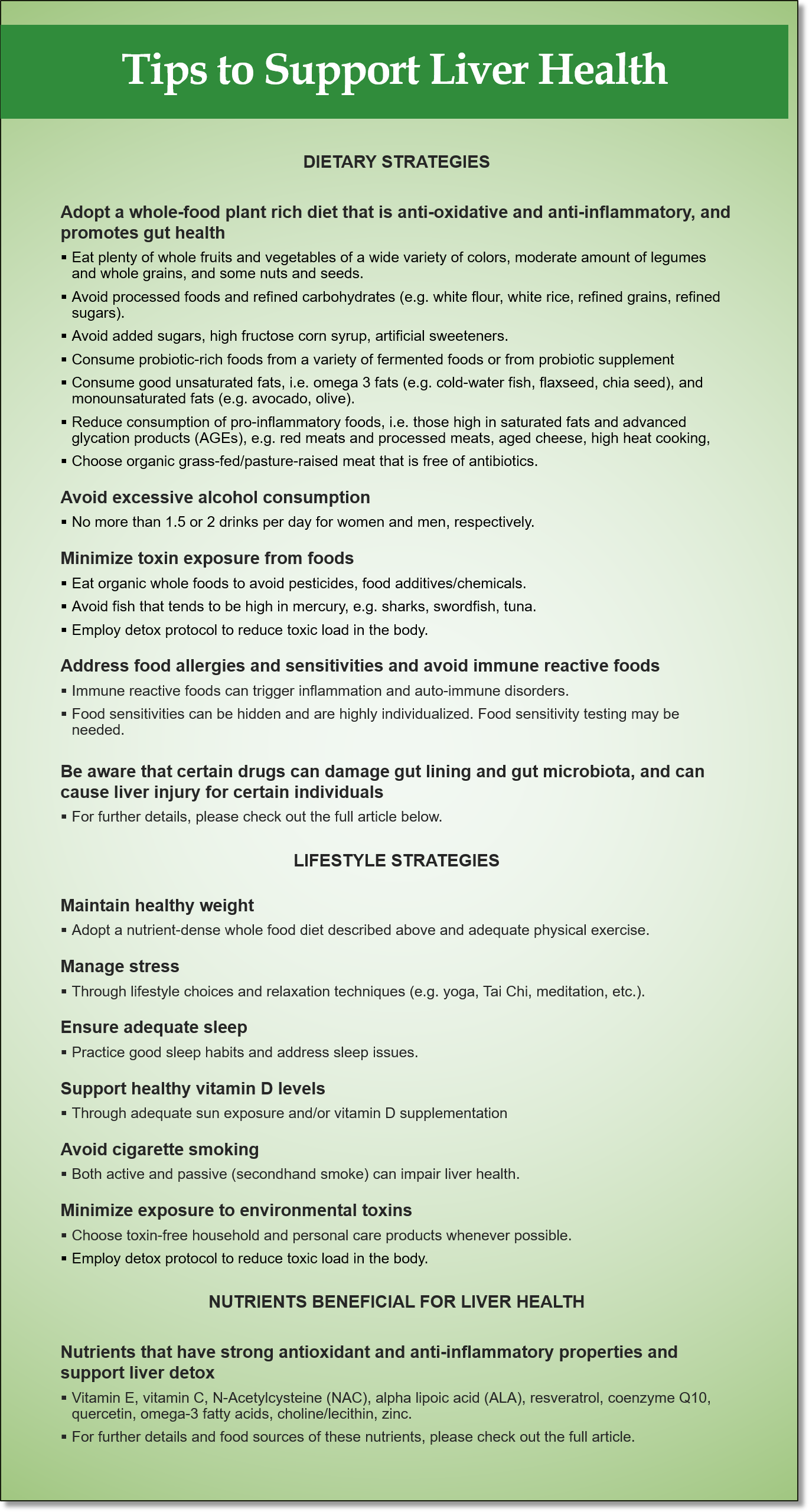
A summary of tips to support liver health through adequate diet, nutrition and lifestyle choices is given below (for more details, see section Tips to Support Liver Health).
Overview of Liver Functions
The vital biological functions carried out in the liver cannot be overstated. More than 500 vital functions have been identified. Some of these functions are listed below:2
- Metabolism of macronutrients (carbohydrates, proteins, fats) that we ingest.
- Regulation of glucose storage and release into blood circulation.
- Regulation of lipid and cholesterol mobilization and balance.
- Regulation of blood levels of amino acids to be used as building blocks of proteins.
- Disposal of nitrogenous waste from protein degradation in the form of urea metabolism (for excretion in the urine).
- Immune defense against pathogens (bacteria, viruses, fungi, parasites, etc.).
- Breakdown and detoxification of toxins, chemicals, excess hormones, and metabolic wastes produced in the body.
- Production of bile that supports fat digestion in the small intestine and stomach acid secretion, and transports broken-down toxins and waste materials into the gastrointestinal (GI) tract for elimination through the colon.
The roles of liver in immune defense are discussed in the next section.
Because of the its many vital functions, liver dysfunction and diseases often lead to many other health conditions and diseases.
Liver and Immunity
With its strategic location in the body, 30% of total blood volume in the body flows and filtered through the liver.3,4
Liver receives blood through the hepatic artery.3,4
Liver also receives blood directly from the GI tract through a blood vessel called the hepatic portal vein. Therefore, liver is the first line of defense against pathogens that enter the blood stream through the GI tract, i.e., pathogens from foods we ingest and pathogens that lives in the gut as part of gut microbiota.3,4
Liver plays important roles in immune surveillance against blood-borne pathogens. Liver contains a large number of immune cells that can mount quick response to invading pathogens.3,4
Failure of the liver to detect or clear blood-borne pathogens can result in systemic infections, often leading to death. In case of liver failure, the primary cause of death is infection.3,4
For overall strategies to support your immune health, please check out my previous article “How to Support Your Immune Health – See What Scientific Research Showed”.
Types of Liver Disease
Liver disease accounts for approximately 2 million deaths per year worldwide.5
Cirrhosis (late-stage liver disease with severe scarring and damage of liver tissue) is the 11th most common cause of death globally.5
In the US, it is estimated that more than 30% of the population has chronic liver disease (CLD).1
Common chronic liver disease includes:
- Alcohol-induced CLD (ALD), caused by excessive alcohol consumption.
- Viral-induced CLD including chronic hepatitis C (CHC) and chronic hepatitis B (CHB).
- Non-alcoholic fatty liver disease (NAFLD), which is associated with metabolic disorders largely due to diet and lifestyle.
- Cholestasis where bile formation and bile flow are impaired.
NAFLD is a spectrum of different degrees of abnormalities in liver tissues, starting from milder condition of fat accumulation in liver cells/tissues (i.e., nonalcoholic fatty liver or NAFL), to inflammation of the liver (i.e., nonalcoholic steatohepatitis, or NASH), and to the more severe scarring/damage of liver tissues (i.e., cirrhosis), liver cancer (i.e., hepatocellular carcinoma), and end-stage liver failure.7
NAFLD is increasingly prevalent especially in Western countries due to diet and lifestyle. NAFLD has emerged to be the leading cause of chronic liver disease and liver transplantation in the US.7
In early stages of NAFLD, i.e., NAFL and NASH, there are usually no signs and symptoms. It can be considered a ‘silent’ disease. Signs and symptoms appear in more advanced stages of the disease, i.e., advanced NASH, cirrhosis and liver cancer.8
Cholestasis can be a consequence of other CLD listed above or can be a primary disease by itself resulted from inflammation and damage of bile ducts. The resultant bile deficiency can have widespread effects in the body due to impaired digestion and absorption, toxin excretion and gut motility.9,10
Risk Factors for Liver Dysfunction and Diseases
In this article, we mainly focus on risk factors associated with the most common non-infection driven CLD, i.e., ALD and NAFLD.
Risk factors associated with primary cholestatic liver diseases are also discussed.
Excessive Alcohol Consumption
Excessive alcohol consumption can lead to ALD including alcoholic fatty liver, alcoholic hepatitis (inflammation of the liver), cirrhosis and end-stage liver disease.7
Genetic, gender, drinking patterns (e.g. drinking with meals reduces the risk compared to drinking on empty stomach) and other lifestyle factors (e.g. cigarette smoking and overweight increases the risk) may influence the tolerable amount and recurring pattern/duration of alcohol consumption that would lead to ALD.11,12
The general recommended alcohol consumption guideline is no more than 20g or 30g equivalence of pure alcohol consumption per day for women and men respectively. In the US, one standard drink is defined as containing 14g equivalence of pure alcohol.13
Metabolic Disorders/Diseases (Obesity, Diabetes, Hypertension, Heart Disease)
The following metabolic syndrome and diseases increase the risk of developing NAFLD:14,15
- Type 2 diabetes (T2D), insulin resistance, high blood glucose level
- Obesity
- Hypertension
- Excess abdominal fat
- High blood triglyceride level
- Low HDL (or good) cholesterol
NAFLD has been reported in over 76% of T2D and 80-90% of obese adults.15
The common underlying disease process among NAFLD and the above metabolic disorders/diseases are chronic inflammation and oxidative stress, which result in dysregulation lipid/cholesterol and glucose metabolism, and liver aberrancy.14,15
NAFLD and metabolic disorders/diseases can form a vicious cycle that potentiates one another.14,15
Gut and Gut Microbiota Dysfunction
As previously discussed, liver receives blood directly from the GI tract through the hepatic portal vein.
Liver is thus exposed to gut pathogens, toxins from foods (e.g. from food additives, pesticides, etc.), endotoxin produced by gut pathogens, and partially- or un-digested food compounds that “leaked” from the gut lumen to the blood stream and subsequently translocated to the liver.16
Translocation of the above unwanted substances occurs when there is aberrancy of the gut lining called intestinal permeability (or leaky gut).16
In addition, gut microbiota imbalance called dysbiosis, i.e., overgrowth of pathogenic microorganisms and undergrowth of beneficial microorganisms in the gut, promotes the translocation of pathogens and pathogen-derived endotoxins to the liver.16
These unwanted substances trigger inflammatory conditions in the liver, leading to NAFLD.16
Dysbiosis also negatively affects the cells of the liver bile ducts, contributing to cholestasis.17
Association has been observed between irritable bowel disease (IBD) (predominantly ulcerative colitis) and primary sclerosing cholangitis (PSC), a cholestatic disease where inflammation and scarring cause narrowing and hardening of bile ducts. Both IBD and PSC are also negatively affected by dysbiosis.10
As bile acids secreted by the liver have protective effects on the gut and gut microbiota, impaired bile acid production and flow due to NAFLD and cholestasis can in turn promote dysbiosis in the gut. Therefore, gut dysbiosis and NAFLD/cholestasis can form a vicious cycle.16
The term gut-liver axis has been introduced in scientific studies to signify the inter-relation and inter-dependency of gut and liver health.16
Industrial Fructose Consumption
The consumption of fructose has skyrocketed in the recent decades due to the use of industrial sweeteners namely high fructose corn syrup (HFCS) and refined sugar or table sugar (sucrose) to processed foods, soft drinks and other sugar-sweetened beverages.18
Sucrose has 50% fructose content while the most common forms of HFCS contain 42% or 55% fructose.18
Based on a report in 2008, US and other Western countries are among the highest consumption of HFCS. The increased consumption of HFCS is suspected to contribute to increased incidence of NAFLD.18
Fructose is metabolized differently in the liver compared to glucose. Here are the detrimental effects of excess fructose consumption:18– 20,51
- Fructose triggers inflammatory response, oxidative stress and lipid formation, which affects both the liver and systemically. High fat and high sugar content of typical Western diets promotes NAFLD and other metabolic syndrome and diseases.
- Fructose impairs energy production in liver cells and causing cell death and scarring, leading to cirrhosis.
- Fructose promotes insulin resistance in both the liver and muscle cells, contributing to high blood glucose levels and T2D.
- Fructose affects gut health by promoting dysbiosis and degradation of gut lining leading to intestinal permeability, both of which contribute to NAFLD and other metabolic syndrome and diseases.
- Fructose affects the brain by promoting a sense of hunger and reduced satiety, thus influencing eating behavior that results in higher calorie consumption.
- There are some similarities between fructose and alcohol metabolism in the liver, both exert similar detrimental health effects.
- Excessive fructose consumption can cause addiction like alcohol and other drugs, also called “fructoholism”.
It is important to distinguish between fructose found in manufactured sweeteners, e.g. HFCS and refined sugar, versus fructose naturally occurring in fruits and some vegetables, in terms of their impact on liver health and metabolic health.23
Whole fruits and vegetables are filled with health-promoting nutrients, antioxidants, fibers and other phytonutrients that help to combat oxidative stress and inflammation, regulate fat metabolism, and promote gut and gut microbiota health; all of which are important for liver health and metabolic health.21
Studies have shown that inclusion of whole fruits in the diet can combat obesity and other metabolic diseases such as T2D and heart disease.21,22
Fruits are rich in phytonutrients called phenolic compounds that have anti-obesity effects. Fruits high in phenolic compounds include blueberry, blackberry, pomegranate, cranberry, plum, and apple.21
Note that it is important to prioritize consumption of whole fresh fruits instead of fruit juice (including those made naturally from fruits) which is void of fiber content, and canned fruits which can contain added sugars/sweeteners.21
In general, a whole food plant-rich diet consisting of plenty of whole fruits and vegetables and void of processed foods and added sugars/sweeteners help to reduce the risk of metabolic diseases (incl. obesity, T2D, hypertension, heart disease), NAFLD and other chronic diseases. See the tips in the section Tips to Support Liver Health.
Toxic Chemical Exposure
Liver is a major detox organ in the body. It is the body’s natural first line of defense against poison and toxins, by filtering and neutralizing harmful substances out of the blood for excretion through the colon.24
Liver is therefore susceptible to injury by chronic exposure to toxin and toxic overload.
Chronic exposure to toxic chemicals throughout the lifetime increases the risk of liver injury and promotes liver disease later in life.24
The detrimental effects can start as early as during the gestational period (i.e. in the mother’s womb) if the mother is exposed to toxic chemicals during pregnancy.24
Liver disease caused by exposures to chemicals has been termed “toxicant-associated fatty liver disease”.24,25
Toxic chemicals can be prevalent in our environment and daily life, including environment pollutants present in the air, water, and soil; and chemicals found in household products, personal care products, building materials, and in the food supplies including chemicals on fruits and vegetables in non-organic farming, and in the food chain (toxic chemicals stored in fatty tissues of animals).25
Toxic chemicals associated with NAFLD include:25–27
- Pesticides (including insecticides, fungicides, herbicides).
- Industrial solvents, more commonly used in industrial and military applications but also has residential usage, for cleaning, degreasing, paint stripping, thinning oil-based plaints, etc.
- Paints, polishes and dyes.
- PCBs and dioxins which are persistent organic pollutants (POPs) that take a long time to breakdown and often accumulate in the food chain, mainly in fatty tissue of animals.
- Chemicals found in fragrance, cosmetics.
- A class of chemicals that disrupt the hormonal (or endocrine) system, called endocrine-disrupting chemicals (EDCs). EDCs not only directly cause liver dysfunction and damage, but also promote other metabolic disorders/diseases such as T2D and obesity, which in turn are risk factors for NAFLD. Some of these EDCs include BPA (found in plastic products and used as protective coating over metals such food cans, metal containers, some exercise equipment, etc.), and PCBs/dioxins.
Cigarette Smoking
Tobacco smoking is a major risk factor for chronic diseases including cancer, and metabolic diseases (heart disease, T2D) which in turns are risk factors for NAFLD.52
Smoking (both active and passive) is also an independent risk factor for advanced fibrosis in patients with primary biliary cirrhosis (PBC), a type of cholestatic disease, and in patients with hepatitis C.52,53
Smoking (both active and passive) is also independently associated with NAFLD.52
Drug-Induced Liver Injury (DILI)
Similar to toxic chemicals, drugs are also chemicals that the liver needs to neutralize for excretion from the body.
When drugs are metabolized in the liver, under certain circumstances may cause liver adaptation and initiate liver injury.28,29
DILI can be patients dependent wherein certain individuals can develop DILI even without exceeding the recommended therapeutic dosage.28,29
Top ranking drugs implicated in causing DILI are, in decreasing order: amoxicillin-clavulanate, flucloxacilllin, atorvastatin, disulfiram, diclofenac, simvastatin, carbamazepine, ibuprofen, erythromycin, and anabolic steroids as bodybuilding agents.28,29
Heavy Metal Exposure
Heavy metals such as arsenic, cadmium, chromium, copper, lead and mercury are environmental pollutants from industrial production that end up in the air, water, soil and food chain.30
Toxic manifestations of heavy metals are attributed to oxidative stress, which affect many organs including liver, brain, kidneys, etc.30
Chronic exposure the heavy metals promote liver aberrancy and NAFLD.30
Vitamin D Deficiency
Vitamin D exerts protective effects on liver cells including anti-inflammatory, anti-fibrotic, and insulin-sensitizing properties.33,35
Vitamin D deficiency has been found to be associated with increased risk of NAFLD.33,35
In addition, vitamin D plays important roles in modulating immune defense against pathogens, hence protecting the liver against viral infections (e.g. hepatitis B, hepatitis C).35
Vitamin D deficiency can be quite prevalent. In the National Health and Nutrition Examination Survey 2005 to 2006 data, the prevalence of vitamin D deficiency (i.e., blood serum 25(OH)D levels < 50 nmol/L) in the United States was found to be 41.6% of the overall population, with increased prevalence among populations with darker skin tones.34
Sleep Issues
Studies have shown that short sleep duration (less than 5 hours), poor sleep quality or sleep disruption, and sleep disorders (e.g. obstructive sleep apnea) are associated with increased risk of developing and progressing of NAFLD.31,32
As detailed in my previous article “Tips for Better Sleep to Support Your Immune Health and Overall Health”, sleep deprivation and disruption have widespread detrimental effects on our health.
These detrimental effects include increased risk of all-cause mortality, overweight and obesity, diabetes, hypertension, high cholesterol, cardiovascular/heart disease, cancers, GI disorders/diseases, cognitive function and memory impairment, Alzheimer’s disease and dementia, and poor mental health, many of which are risk factors for NAFLD.
Tips to Support Liver Health
Our diet and lifestyle play important roles in mitigating the risk factors associated with CLD.
Some tips for diet and lifestyle choices are provided below, as well as certain nutrients and nutritional compounds that are specifically beneficial for liver health.
Dietary Choices to Support Liver Health
Diets that reduce oxidative stress, chronic inflammation, risks of metabolic disorders/diseases and toxin exposure, and support gut and gut microbiota health are beneficial for liver health.
Adopt a whole-food plant rich diet that is anti-oxidative and anti-inflammatory, and promote gut and gut microbiota health
- Eat plenty of whole fruits and vegetables of a wide variety of colors, moderate amount of legumes and whole grains, and some nuts and seeds. Such diets are rich in a wide range of antioxidants, fibers, prebiotics and other health promoting micronutrients and phytonutrients, which help to combat oxidative stress, promote anti-inflammatory response, regulate blood sugar and support gut health. Leafy greens, cruciferous vegetables, and berries are particularly beneficial.
- Avoid or minimize consumption of refined carbohydrates such as white flour, white rice, refined grains, added sugars, HFCS, and sweeteners.
- Avoid or minimize consumption of processed foods and artificial sweeteners.
- Consume probiotic-rich foods from a variety of fermented foods or from probiotic supplement.
- Consume a high ratio of unsaturated fats including monounsaturated fats (e.g. olive, avocado) and omega-3 polyunsaturated fats (e.g. cold-water fish, flaxseed, chia seed, some nuts) over saturated fats.
- Minimize or reduce consumption of foods high in saturated fats and advanced glycation products (AGEs) such as meats (especially red meats and processed meats), foods cooked in high/dry heat, and dairy products especially aged cheese.
- Choose organic, grass-fed/pasture-raised meat that is free of antibiotics.
Avoid excessive alcohol consumption
- No more than 20g or 30g equivalence of pure alcohol consumption (approximately 1.5 or 2 drinks) per day for women and men, respectively.
Minimize toxin exposure from foods
- Avoid toxins in foods including pesticides, herbicides, food additives, chemicals, by choosing organic whole foods whenever possible
- Avoid fish that tend to be high in mercury, e.g. sharks, swordfish, tuna.
- Employ detox protocol to reduce toxic load in the body.
Address food allergies and sensitivities and avoid immune reactive foods
- Immune reactive foods can contribute to autoimmunity and inflammation.
- Food allergies and sensitivities can be hidden and are highly individualized. Food sensitivity testing may be needed.
Be aware that certain drugs can damage gut lining and gut microbiota
- These include antibiotics, NSAIDs, proton pump inhibitors (PPIs), and osmotic laxatives.
Be aware that certain drugs can incur liver injury for certain individuals
- These include amoxicillin-clavulanate, flucloxacilllin, atorvastatin, disulfiram, diclofenac, simvastatin, carbamazepine, ibuprofen, erythromycin, and anabolic steroids as bodybuilding agents.
Further information on guidelines for healthy eating can be found in: Simple Guidelines for Healthy Eating, Are Carbs and Sugars All Bad.
Further information on gut health can be found in: Why Your Gut Feeling Matters, You are What You Eat? Not Quite.
Lifestyle Choices to Support Liver Health
Lifestyle that reduce oxidative stress, chronic inflammation, risks of metabolic disorders/diseases and toxin exposure are beneficial for liver health.
Such lifestyle practices include:
- Adopt healthy weight management through nutrient-dense whole food diets (see above) and adequate physical exercise.
- Support healthy vitamin D levels through adequate sun exposure and/or vitamin D supplementation.
- Avoid cigarette smoking (both active and passive).
- Minimize exposure environmental toxins by choosing toxin-free household and personal care products whenever possible. Employ detox protocol to reduce toxic load in the body.
- Ensure adequate sleep by practicing good sleep habits and addressing sleep issues. See details in “Tips for Better Sleep to Support Your Immune Health and Overall Health”.
- Adopt stress management techniques such as yoga, Tai Chi, meditation, low-intensity exercise, music therapy, etc.
Specific Nutrients and Nutritional Compounds That Support Liver Health
Nutrients and nutritional compounds that exert strong antioxidant and anti-inflammatory properties and support liver detox are generally beneficial for liver health.
Some of them are listed here:
Vitamin E
Vitamin E is an antioxidant and has been used in the treatment of NAFLD.37
Vitamin E can significantly improve liver function and liver tissue/cell structure.37
Food sources of vitamin E include leafy greens, broccoli, sunflower seeds, almonds, avocado, etc.
Vitamin C
Vitamin C is also an antioxidant and it works synergistically with other liver-protective antioxidants such as vitamin E and NAC (see below).
Low dietary vitamin C intake was found to be associated with increased risk of NAFLD.39
Vitamin C supplementation was found to have protective effect on NAFLD-related liver damage.38
Food sources of vitamin C include fruits and vegetables although heat in cooking destroy vitamin C.
N-Acetylcysteine (NAC)
NAC is a supplement form of cysteine, an amino acid that is found in most high-protein foods, e.g. meat, eggs, legumes, seeds, etc.
NAC exerts antioxidative, anti-inflammatory, and liver protective properties and acts as precursor of glutathione, which is one of the most potent antioxidant and detox agent synthesized naturally in the body.36
NAC therapy has be used to treat patients with acute liver failure, cirrhosis and DILI.36
Alpha Lipoic Acid (ALA)
ALA is a natural antioxidant synthesized in the liver and other tissues.42
ALA has strong antioxidant properties. In addition, ALA can recycle/regenerate other antioxidants including vitamin C and vitamin E. ALA can also recycle/regenerate glutathione and restore glutathione reserve in the body.42
ALA can also act as chelator for heavy metals, facilitating their detoxification, thus reducing the toxic load in the liver.42
ALA can stimulate insulin sensitivity and induce blood glucose level reduction, thus mitigating one of the risk factors of NAFLD.42
ALA supplementation was found the improve biomarkers associated with NAFLD.43
Although ALA is synthesized in the body, there are also natural food sources of ALA including organ meats, grass-fed beef, broccoli, spinach and brussel sprouts.
Resveratrol
Resveratrol is a phytonutrient found in certain fruits and nuts.
Resveratrol has antioxidant and anti-inflammatory properties and can inhibit lipid accumulation in the body.44
Studies have shown that resveratrol supplementation can reduce blood pressure, thus mitigating one of the risk factors of NAFLD.
However, studies using resveratrol supplementation as treatment for NAFLD have shown conflicting results, where some studies showed beneficial effects while other studies did not show any difference.44
Food sources of resveratrol include red grapes, blueberries, raspberries, mulberries, strawberries, peanuts, and dark chocolate.
Coenzyme Q10 (CoQ10)
CoQ10 is a ubiquitous compound found in cell membranes and in the energy production center (i.e. the mitochondria) within a cell.46
CoQ10 plays important roles in energy metabolism. CoQ10 also exerts strong antioxidant and anti-inflammatory properties. CoQ10 can inhibit formation of fat cells.46
CoQ10 is synthesized naturally in the body. There are also food sources of CoQ10. Food sources of CoQ10 become important when there is CoQ10 deficiency associated with certain chronic diseases (e.g., heart disease, muscular dystrophy, Alzheimer’s disease etc.) and the use of statin, a cholesterol lowering drug.46
CoQ10 supplementation was found to be beneficial for the management metabolic disorders/diseases including hypertension, heart disease, insulin resistance/T2D, high triglycerides, high LDL cholesterol and low HDL cholesterol; all of which are risk factors for NAFLD.46
CoQ10 supplementation was found to improve biomarkers associated with NAFLD.46
Food sources of CoQ10 include meat, fatty fish, spinach, cauliflower, broccoli, strawberries, peanuts, sesame seeds, pistachios.
Quercetin
Quercetin is a phytonutrient belonging to the flavonoid group and is found in some fruits and vegetables.47
Quercetin exhibits antioxidant, anti-inflammatory, anti-diabetic, and cardiovascular-protective effects, all of which help to mitigate risk factors of NAFLD.47
Quercetin also increases the body’s antioxidant capacity by support the regeneration of glutathione.48
Quercetin was shown to prevent fat accumulation in the liver and liver injury due to chronic excessive alcohol consumption.47
Quercetin was also shown to protect liver against injury from toxicity.48
Food sources of quercetin include grapes, berries, cherries, apples, citrus fruits, onions, buckwheat, kale, tomatoes, red wine, and black tea.
Omega-3 Fatty Acids
Omega-3 fatty acids exert anti-inflammatory properties and have been shown to reduce fat accumulation in the liver.41
Food sources of omega-3 fatty acids include cold-water fatty fish, flaxseed, chia seed, and some nuts.
Choline and Lecithin
Choline is an essential nutrient for the body.
Choline is a precursor to phosphatidylcholine, an important constituent of cellular membranes, bile, lipoproteins (important for fat and cholesterol transport), and neurotransmitter.40
Diet low in choline can lead to fat accumulation in the liver and NAFLD. 40
Most choline in the diet is derived from lecithin. Lecithin contains both choline and phosphatidylcholine.
Food sources of choline and lecithin include organ meats, eggs, soy, sunflower seeds, nuts, dairy, cauliflower, and broccoli.
Zinc
Zinc is an essential trace mineral required for normal cell function and development. It is also a critical component of many zinc proteins/enzymes.49
Liver is the main organ for zinc metabolism, which can be impaired in case of liver disease.50
Zinc deficiency and altered metabolism have been observed in many types of liver disease, including ALD, viral liver disease, and cirrhosis.49
On the other hand, zinc deficiency can alter liver cell functions, impair cell repair and regeneration, promote inflammatory response, and induce oxidative stress and damage.50
Therefore, liver disease and zinc deficiency can form a vicious cycle.
Zinc supplementation can counter the above vicious cycle and negative effects of zinc deficiency. Zinc supplementation has been shown to improve liver function in ALD and hepatitis C and improve patient outcomes in liver cirrhosis.49,50
Food sources of zinc include shellfish especially oyster and crab, beef, white meats, beans, pumpkin seeds, and some nuts.
Related Articles
How to Support Your Immune Health – See What Scientific Research Showed
Tips for Better Sleep to Support Your Immune Health and Overall Health
Simple Guidelines for Healthy Eating
You are What You Eat? Not Quite
References
-
- American Liver Foundation. Liver Disease Statistics. American Liver Foundation. https://liverfoundation.org/liver-disease-statistics/. Published 2017.
- Trefts E, Gannon M, Wasserman DH. The liver. Curr Biol. 2017;27(21):R1147-R1151. doi:10.1016/j.cub.2017.09.019
- Jenne CN, Kubes P. Immune surveillance by the liver. Nat Immunol. 2013;14(10):996-1006. doi:10.1038/ni.2691
- Kubes P, Jenne C. Immune Responses in the Liver. Annu Rev Immunol. 2018;36:247-277. doi:10.1146/annurev-immunol-051116-052415
- Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70(1):151-171. doi:10.1016/j.jhep.2018.09.014
- Marcellin P, Kutala BK. Liver diseases: A major, neglected global public health problem requiring urgent actions and large-scale screening. Liver Int. 2018;38 Suppl 1:2-6. doi:10.1111/liv.13682
- Udompap P, Kim D, Kim WR. Current and Future Burden of Chronic Nonmalignant Liver Disease. Clin Gastroenterol Hepatol. 2015;13(12):2031-2041. doi:10.1016/j.cgh.2015.08.015
- National Institute of Diabetes and Digestive and Kidney Diseases. Nonalcoholic Fatty Liver Disease & NASH. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash. Published 2020.
- Jüngst C, Berg T, Cheng J, et al. Intrahepatic cholestasis in common chronic liver diseases. Eur J Clin Invest. 2013;43(10):1069-1083. doi:10.1111/eci.12128
- Jansen PL, Ghallab A, Vartak N, et al. The ascending pathophysiology of cholestatic liver disease. Hepatology. 2017;65(2):722-738. doi:10.1002/hep.28965
- Stickel F, Datz C, Hampe J, Bataller R. Pathophysiology and Management of Alcoholic Liver Disease: Update 2016 [published correction appears in Gut Liver. 2017 May 15;11(3):447]. Gut Liver. 2017;11(2):173-188. doi:10.5009/gnl16477
- Campollo O. Alcohol and the Liver: The Return of the Prodigal Son. Ann Hepatol. 2019;18(1):6-10. doi:10.5604/01.3001.0012.7854
- European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu; European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of alcohol-related liver disease. J Hepatol. 2018;69(1):154-181. doi:10.1016/j.jhep.2018.03.018
- Pappachan JM, Babu S, Krishnan B, Ravindran NC. Non-alcoholic Fatty Liver Disease: A Clinical Update. J Clin Transl Hepatol. 2017;5(4):384-393. doi:10.14218/JCTH.2017.00013
- Al-Dayyat HM, Rayyan YM, Tayyem RF. Non-alcoholic fatty liver disease and associated dietary and lifestyle risk factors. Diabetes Metab Syndr. 2018;12(4):569-575. doi:10.1016/j.dsx.2018.03.016
- Albhaisi SAM, Bajaj JS, Sanyal AJ. Role of gut microbiota in liver disease. Am J Physiol Gastrointest Liver Physiol. 2020;318(1):G84-G98. doi:10.1152/ajpgi.00118.2019
- LaRusso NF, Tabibian JH, O’Hara SP. Role of the Intestinal Microbiome in Cholestatic Liver Disease. Dig Dis. 2017;35(3):166-168. doi:10.1159/000450906
- Alwahsh SM, Gebhardt R. Dietary fructose as a risk factor for non-alcoholic fatty liver disease (NAFLD). Arch Toxicol. 2017;91(4):1545-1563. doi:10.1007/s00204-016-1892-7
- Lustig RH. Fructose: it’s “alcohol without the buzz”. Adv Nutr. 2013;4(2):226-235. Published 2013 Mar 1. doi:10.3945/an.112.002998
- Stanhope KL. Sugar consumption, metabolic disease and obesity: The state of the controversy. Crit Rev Clin Lab Sci. 2016;53(1):52-67. doi:10.3109/10408363.2015.1084990
- Sharma SP, Chung HJ, Kim HJ, Hong ST. Paradoxical Effects of Fruit on Obesity. Nutrients. 2016;8(10):633. Published 2016 Oct 14. doi:10.3390/nu8100633
- Madero M, Arriaga JC, Jalal D, et al. The effect of two energy-restricted diets, a low-fructose diet versus a moderate natural fructose diet, on weight loss and metabolic syndrome parameters: a randomized controlled trial. Metabolism. 2011;60(11):1551-1559. doi:10.1016/j.metabol.2011.04.001
- Petta S, Marchesini G, Caracausi L, et al. Industrial, not fruit fructose intake is associated with the severity of liver fibrosis in genotype 1 chronic hepatitis C patients. J Hepatol. 2013;59(6):1169-1176. doi:10.1016/j.jhep.2013.07.037
- Treviño LS, Katz TA. Endocrine Disruptors and Developmental Origins of Nonalcoholic Fatty Liver Disease. Endocrinology. 2018;159(1):20-31. doi:10.1210/en.2017-00887
- Al-Eryani L, Wahlang B, Falkner KC, et al. Identification of Environmental Chemicals Associated with the Development of Toxicant-associated Fatty Liver Disease in Rodents. Toxicol Pathol. 2015;43(4):482-497. doi:10.1177/0192623314549960
- Heindel JJ, Blumberg B, Cave M, et al. Metabolism disrupting chemicals and metabolic disorders. Reprod Toxicol. 2017;68:3-33. doi:10.1016/j.reprotox.2016.10.001
- Foulds CE, Treviño LS, York B, Walker CL. Endocrine-disrupting chemicals and fatty liver disease. Nat Rev Endocrinol. 2017;13(8):445-457. doi:10.1038/nrendo.2017.42
- Teschke R. Top-ranking drugs out of 3312 drug-induced liver injury cases evaluated by the Roussel Uclaf Causality Assessment Method. Expert Opin Drug Metab Toxicol. 2018;14(11):1169-1187. doi:10.1080/17425255.2018.1539077
- Teschke R. Idiosyncratic DILI: Analysis of 46,266 Cases Assessed for Causality by RUCAM and Published From 2014 to Early 2019. Front Pharmacol. 2019;10:730. Published 2019 Jul 23. doi:10.3389/fphar.2019.00730
- García-Niño WR, Pedraza-Chaverrí J. Protective effect of curcumin against heavy metals-induced liver damage. Food Chem Toxicol. 2014;69:182-201. doi:10.1016/j.fct.2014.04.016
- Wijarnpreecha K, Thongprayoon C, Panjawatanan P, Ungprasert P. Short sleep duration and risk of nonalcoholic fatty liver disease: A systematic review and meta-analysis. J Gastroenterol Hepatol. 2016;31(11):1802-1807. doi:10.1111/jgh.13391
- Marin-Alejandre BA, Abete I, Cantero I, et al. Association between Sleep Disturbances and Liver Status in Obese Subjects with Nonalcoholic Fatty Liver Disease: A Comparison with Healthy Controls. Nutrients. 2019;11(2):322. Published 2019 Feb 2. doi:10.3390/nu11020322
- Barchetta I, Cimini FA, Cavallo MG. Vitamin D Supplementation and Non-Alcoholic Fatty Liver Disease: Present and Future. Nutrients. 2017;9(9):1015. Published 2017 Sep 14. doi:10.3390/nu9091015
- Forrest KY, Stuhldreher WL. Prevalence and correlates of vitamin D deficiency in US adults. Nutr Res. 2011;31(1):48–54. doi:10.1016/j.nutres.2010.12.001
- Keane JT, Elangovan H, Stokes RA, Gunton JE. Vitamin D and the Liver-Correlation or Cause?. Nutrients. 2018;10(4):496. Published 2018 Apr 16. doi:10.3390/nu10040496
- Heil J, Schultze D, Schemmer P, Bruns H. N-acetylcysteine protects hepatocytes from hypoxia-related cell injury. Clin Exp Hepatol. 2018;4(4):260-266. doi:10.5114/ceh.2018.80128
- Sato K, Gosho M, Yamamoto T, et al. Vitamin E has a beneficial effect on nonalcoholic fatty liver disease: a meta-analysis of randomized controlled trials. Nutrition. 2015;31(7-8):923-930. doi:10.1016/j.nut.2014.11.018
- Ivancovsky-Wajcman D, Fliss-Isakov N, Salomone F, et al. Dietary vitamin E and C intake is inversely associated with the severity of nonalcoholic fatty liver disease. Dig Liver Dis. 2019;51(12):1698-1705. doi:10.1016/j.dld.2019.06.005
- Wei J, Lei GH, Fu L, Zeng C, Yang T, Peng SF. Association between Dietary Vitamin C Intake and Non-Alcoholic Fatty Liver Disease: A Cross-Sectional Study among Middle-Aged and Older Adults. PLoS One. 2016;11(1):e0147985. Published 2016 Jan 29. doi:10.1371/journal.pone.0147985
- Mehedint MG, Zeisel SH. Choline’s role in maintaining liver function: new evidence for epigenetic mechanisms. Curr Opin Clin Nutr Metab Care. 2013;16(3):339-345. doi:10.1097/MCO.0b013e3283600d46
- Scorletti E, Byrne CD. Omega-3 fatty acids and non-alcoholic fatty liver disease: Evidence of efficacy and mechanism of action. Mol Aspects Med. 2018;64:135-146. doi:10.1016/j.mam.2018.03.001
- Tibullo D, Li Volti G, Giallongo C, et al. Biochemical and clinical relevance of alpha lipoic acid: antioxidant and anti-inflammatory activity, molecular pathways and therapeutic potential. Inflamm Res. 2017;66(11):947-959. doi:10.1007/s00011-017-1079-6
- Hosseinpour-Arjmand S, Amirkhizi F, Ebrahimi-Mameghani M. The effect of alpha-lipoic acid on inflammatory markers and body composition in obese patients with non-alcoholic fatty liver disease: A randomized, double-blind, placebo-controlled trial. J Clin Pharm Ther. 2019;44(2):258-267. doi:10.1111/jcpt.12784
- Zhang C, Yuan W, Fang J, et al. Efficacy of Resveratrol Supplementation against Non-Alcoholic Fatty Liver Disease: A Meta-Analysis of Placebo-Controlled Clinical Trials. PLoS One. 2016;11(8):e0161792. Published 2016 Aug 25. doi:10.1371/journal.pone.0161792
- Fogacci F, Tocci G, Presta V, Fratter A, Borghi C, Cicero AFG. Effect of resveratrol on blood pressure: A systematic review and meta-analysis of randomized, controlled, clinical trials. Crit Rev Food Sci Nutr. 2019;59(10):1605-1618. doi:10.1080/10408398.2017.1422480
- Martelli A, Testai L, Colletti A, Cicero AFG. Coenzyme Q10: Clinical Applications in Cardiovascular Diseases. Antioxidants (Basel). 2020;9(4):341. Published 2020 Apr 22. doi:10.3390/antiox9040341
- Salehi B, Machin L, Monzote L, et al. Therapeutic Potential of Quercetin: New Insights and Perspectives for Human Health. ACS Omega. 2020;5(20):11849-11872. Published 2020 May 14. doi:10.1021/acsomega.0c01818
- Xu D, Hu MJ, Wang YQ, Cui YL. Antioxidant Activities of Quercetin and Its Complexes for Medicinal Application. Molecules. 2019;24(6):1123. Published 2019 Mar 21. doi:10.3390/molecules24061123
- Mohammad MK, Zhou Z, Cave M, Barve A, McClain CJ. Zinc and liver disease [published correction appears in Nutr Clin Pract. 2012 Apr;27(2):305. Mohommad, Mohammad K [corrected to Mohammad, Mohammad K]]. Nutr Clin Pract. 2012;27(1):8-20. doi:10.1177/0884533611433534
- Grüngreiff K, Reinhold D, Wedemeyer H. The role of zinc in liver cirrhosis. Ann Hepatol. 2016;15(1):7-16. doi:10.5604/16652681.1184191
- Ribeiro A, Igual-Perez MJ, Santos Silva E, Sokal EM. Childhood Fructoholism and Fructoholic Liver Disease. Hepatol Commun. 2018;3(1):44-51. Published 2018 Nov 30. doi:10.1002/hep4.1291
- Liu Y, Dai M, Bi Y, et al. Active smoking, passive smoking, and risk of nonalcoholic fatty liver disease (NAFLD): a population-based study in China. J Epidemiol. 2013;23(2):115-121. doi:10.2188/jea.je20120067
- Mantaka A, Koulentaki M, Samonakis D, et al. Association of smoking with liver fibrosis and mortality in primary biliary cholangitis. Eur J Gastroenterol Hepatol. 2018;30(12):1461-1469. doi:10.1097/MEG.0000000000001234
