You may have heard of the phrase “You Are What You Eat”. It is true that the foods that we eat has a big impact on our health and wellbeing, as shown by numerous scientific studies. Please check out my previous blogs on Diets and Chronic Diseases on how certain diets can reduce the risks of many chronic diseases.
However, our food intake is only part of the story. The foods that we consume have to be properly digested and absorbed into our body by our digestive system or our gut. Once absorbed, the corresponding nutrients have to be properly metabolized to be fully utilized for our body functions.
So, the more accurate phrase should be “You are what you eat, digest, absorb and metabolize”.
Any disruption or dysfunction in any of the above processes could render the seemingly healthy and nutritious foods and even the so-called superfoods that we eat to be futile.
Let’s take a closer look at each of these complex processes and find out more on how you can better support your health and wellbeing.
Foods and Diets
The foods we eat provide the building blocks for our body to generate energy, repair damaged cells and tissues, generate and regenerate new cells and tissues, and to support normal body functions of our various organ systems such as digestive system, immune system, brain and nervous system, cardiovascular system, hormonal/endocrine system, etc.
Therefore, to best support our body, it makes sense to consume nutrient-dense foods that are void of toxins, whenever possible.
However, the various dietary recommendations (e.g. low carb diet, low fat diet, Paleo diet, ketogenic diet, etc.) and associated health claims can be confusing and sometime contradictory to one another.
I have previously put together an article “Simple Guidelines of Health Eating”, which summarized some general guidelines for healthy eating, backed by evidenced-based scientific studies which showed that such healthy eating practice can reduce the risk of many of the dreaded chronic diseases including type 2 diabetes, high blood pressure, heart disease, Alzheimer’s disease and dementia, and cancers.
Please also check out my previous blog “Are Carbs and Sugars all Bad” which provided a detailed look into different types of carbs and why not all carbs are created equal. Some discussion on two recently popular low carbs diets, i.e., Paleo diet and ketogenic diet, are also included in this blog.
Digestion and Absorption
“All diseases begin in the gut” ~Hippocrates
Hippocrates, a Greek physician who lived more than 2000 years ago and widely regarded as the father of modern medicine, believed that all diseases begin in the gut.
It is interesting to note that such claim has increasingly been supported by modern scientific research.
We could eat the most nutritious foods, but if our digestion and absorption functions are compromised, the health promoting nutrients cannot be absorbed and utilized in our body.
Digestion mostly occurs in the stomach and the proximal part of the small intestine, while absorption mostly occurs in the proximal part of the small intestine.
Some common factors affecting digestion and absorption functions are described in the sections below (see Figure 1).
For a more detailed look at how the health of our gut affects not only our digestion and absorption function but also the health of our body as a whole (ranging from immune system, brain and nervous system, cardiovascular system, glucose metabolism, skin, and many more), please check out my previous article “Why Your Gut Feeling Matters”.
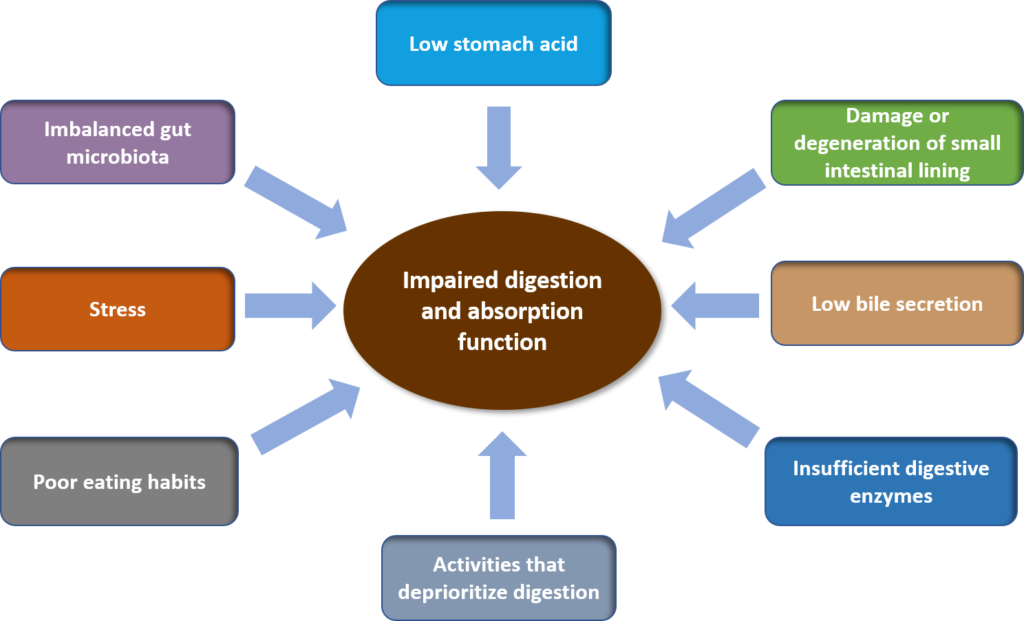
Figure 1. Multifactorial influence on digestion and absorption function
Low Stomach Acid
Low stomach acid contributes to maldigestion of protein, malabsorption of vitamin B12, and acid reflux/heart burn (GERD – gastroesophageal reflux disease).
Some of the contributing factors to low stomach acid include:1
- pylori infection.
- Low bile (due to liver and gallbladder dysfunction).
- Zinc and sodium deficiency.
- Prolonged use of certain drugs including antacids, NSAIDs (non-steroidal anti-inflammatory drugs).
Damage and Degeneration of the Lining of Small intestine
This contributes to maldigestion and malabsorption of various nutrients, because the internal lining (or mucosal barrier) of proximal part of the small intestine is where most digestion and absorption action occurs.
Some contributing factors to the damage and degeneration of mucosal barrier include:2–5
- Toxins in foods including pesticides, herbicides, heavy metals, food additives, chemicals, environmental pollutants.
- Gut infections (including bacteria, virus, parasites).
- Chronic inflammation of the gut including Celiac disease, irritable bowel disease (IBD) including Crohn’s disease and ulcerative colitis.
- Consumption of certain reactive or sensitive foods, such as gluten etc., which is unique to each person.
- Alcohol consumption.
- Diets low in fiber, high in refined sugar and fructose, and high in saturated fats.
- Imbalanced gut microbiota or dysbiosis.
- Certain drugs including antibiotics, NSAIDs and proton pump inhibitors (PPIs)
- Stress.
Low Bile Secretion
Low bile secretion into the small intestine contributes to maldigestion and malabsorption of fats and impaired secretion of stomach acid.
Contributing factors to low bile secretion include:
- Missing or congested gallbladder (e.g. due to gallstone).
- Liver disorders such as cystic fibrosis, hepatitis.
- Liver stress that results in impaired secretion and stagnation of bile (see further discussion of liver stress below).
- Malabsorption and poor recovery of bile in the small intestine due to IBD, chronic malabsorption, and chronic diarrhea.
Liver stress can be quite common in our modern lifestyle, due to toxin build-up from our foods and environment that overtax the liver. Such toxins include pesticides and herbicides, food additives, chemicals from personal care and household products and environmental exposure, heavy metals (e.g. mercury from fish and amalgam filling, aluminum in cookware, etc.).24,25
Other contributing factors to liver stress include excessive alcohol consumption, parasite infection, and certain drugs such an antibiotics and chemotherapy drugs.22,23,26
Insufficient Digestive Enzymes
Digestive enzymes are secreted throughout the digestive tract to digest macronutrients (carbohydrates, proteins, fats) starting at the mouth, and continue on to the stomach and subsequently to the small intestine.
Major digestion action by digestive enzymes occur at the proximal part of the small intestine. These digestive enzymes are secreted by the pancreas and cells of the small intestine mucosal barrier.
As discussed above, damage and degeneration of the mucosal barrier impair the secretion of digestive enzymes.
In addition, impaired pancreatic enzyme secretion, also known as exocrine pancreatic insufficiency (EPI) is a major cause of maldigestion and malabsorption.6
Contributing factors to EPI include:6
- Diseases of the pancreas such as pancreatitis, cystic fibrosis, pancreatic cancer, etc. are the most common causes.
- Other health conditions including type 1 and type 2 diabetes, and gut related disorders including Celiac disease, IBD (Crohn’s disease, ulcerative colitis) and small intestine bacteria overgrowth (SIBO).
- Aging, which may play a role in the decline of pancreatic enzyme secretion.
Imbalanced Gut Microbiota
Imbalanced gut microbiota or dysbiosis is the overgrowth of bad (pathogenic) microbes and undergrowth of good (symbiotic) microbes in our gut.
There is an estimated 10 to 100 trillion microbes reside in the digestive track, outnumbering the number of cells in the human body. In addition, microbiome contains approximately 100x more genes than the human genome.7,8
Symbiotic microbes play important roles in digestion and metabolism functions of human body. Specifically for digestion, the important roles of symbiotic microbes include:8–10
- Digestion of certain carbohydrates, such as xyloglucans found in certain vegetables and indigestible dietary fibers, into important nutrients for the health of the gut and the body as a whole.
- Protection of digestive tract from pathogen colonization.
- Nourishment and regeneration of intestinal mucosal barrier
Contributing factors to an imbalanced gut microbiota include:11,12
- Diet high in processed foods, artificial sweeteners, and low in fibers and prebiotics.
- Use of certain drugs including osmotic laxatives, PPIs, antibiotics.
- Exposure to agricultural antibiotics found in animal food products.
- Mode of delivery during childbirth, i.e. assisted delivery instead of natural childbirth.
- Formula fed instead of breast fed for infants.
- Stress.
Stress
The impact of stress on digestion function is multi-fold. As previously described, stress can contribute to imbalanced gut microbiota and damage/degeneration of small intestine mucosal barrier.
In addition, stress induces fight-or-flight response in the body, which activates the sympathetic nervous system (SNS) and trigger the release of cortisol (the stress hormone), while suppressing the parasympathetic nervous system (PNS).
SNS and cortisol drive blood flow to carry oxygen and nutrients to major organs, including the brain, skeletal muscles, heart to prepare for fight-or-flight. When this happens, PNS-triggered rest and restoration functions of the body including digestion and elimination, cell and tissue repair are deprioritized.13
Activities That Deprioritize Digestion
Activities that affect digestion are those that activate the stress response in the body or redirect blood flow away of the digestive organs. This can range from eating at your desk while working or in a meeting, eating in a rush, in a stressful situation, or with an anxious state of mind, to even light exercise such as walking soon after eating.
It is good to allow yourself to rest and digest for at least half an hour to one hour after a meal before engaging in light to moderate activities.
Poor Eating Habits
There are some common eating habits that can impair digestion.
Eating in a rush and not chewing our foods properly are common habits. Chewing stimulates the secretion of saliva which contains digestive enzyme. Chewing also stimulates the secretion of stomach acid.
As discussed above, multitasking while eating (e.g. working, watching TV, etc.) is also a common habit.
Drinking too much fluid shortly before, after or during eating can dilute stomach acid and impair digestion.
Metabolism
Metabolism is the sum of all biochemical processes occurring within a living cell or organism that are necessary for the maintenance of life.
The nutrients that are absorbed into our body have to be properly metabolized to support the various body functions.
Without being exhaustive, we provide here some examples of important metabolic processes.
Energy Production and Mitochondria
Glucose that enters the body through digestion and absorption of carbohydrates has to be metabolized into energy in order to be useful to cells in the body. There is one or more energy production entity in each cell called mitochondria (except for red blood cells which do not have mitochondria).
Mitochondria is a cell’s powerhouse. In addition, mitochondria play crucial roles in many essential cellular functions. Therefore, proper functioning of mitochondria in each cell is crucial for our health. However, many factors can contribute to mitochondria dysfunction including toxins (incl. heavy metals, pesticides/herbicides, chemicals, environmental pollutants), certain drugs, chronic infection, oxidative stress. chronic inflammation, stress, etc.14,15
The research on mitochondria functions and dysfunction has gained tremendous interest in medical sciences in the last 20 years.16 In addition to lack of energy such as chronic fatigue syndrome, mitochondria dysfunction has been associated with many chronic degenerative diseases including neurodegenerative diseases (incl Parkinson’s, Alzheimer’s), metabolic disorders (incl diabetes, heart disease, obesity, hypertension), cancers, etc.17
Roles of Microbiota in Metabolism
Our gut microbiota plays important roles in providing certain metabolic functions that otherwise would not have been possible. These include:8,9
- Salvaging undigestible carbohydrates, especially complex long-chain carbohydrates, into short-chain fatty acids (SCFAs). SCFAs serve as important energy source for the mucosal cells of the colon and promote healthy intestinal lining. SCFAs are also used in other body functions including turning on anti-inflammatory response and supporting mitochondria function.
- Synthesis of vitamins including folate, thiamine, biotin, riboflavin, pantothenic acid and vitamin K. It is estimated that half of daily vitamin K requirement is provided by gut bacteria.
- Synthesis of certain essential amino acids from carbohydrates, instead of through ingested protein.
- Lipid metabolism.
- Deconjugation of bile salts.
The important roles gut microbiota play in our health can be reflected in the many chronic diseases and disorders associated with imbalanced gut microbiota. These include:9,18–21
- Obesity
- Metabolic disorders
- Nonalcoholic fatty liver disease
- Nonalcoholic steatohepatitis
- Type 2 diabetes
- Irritable bowel syndrome
- IBD
- Colorectal cancer
- Cognitive/psychiatric/neurological disorders such as autism spectrum disorders, anxiety, depression, schizophrenia, and Parkinson’s disease.
Hence, having a healthy gut microbiota is crucial and cannot be overlooked.
Related Articles
Simple Guidelines of Health Eating
References
- Anand B S. Peptic ulcer disease. http://emedicine.medscape.com/article/181753-overview#a3. Published 2015.
- Mu Q, Kirby J, Reilly CM, Luo XM. Leaky Gut As a Danger Signal for Autoimmune Diseases. Front Immunol. 2017;8:598. Published 2017 May 23. doi:10.3389/fimmu.2017.00598
- Hollon J, Puppa EL, Greenwald B, Goldberg E, Guerrerio A, Fasano A. Effect of gliadin on permeability of intestinal biopsy explants from celiac disease patients and patients with non-celiac gluten sensitivity. Nutrients. 2015;7(3):1565-76. Published 2015 Feb 27. doi:10.3390/nu7031565
- König J, Wells J, Cani PD, et al. Human Intestinal Barrier Function in Health and Disease. Clin Transl Gastroenterol. 2016;7(10):e196. Published 2016 Oct 20. doi:10.1038/ctg.2016.54
- Bischoff SC, Barbara G, Buurman W, et al. Intestinal permeability–a new target for disease prevention and therapy. BMC Gastroenterol. 2014;14:189. Published 2014 Nov 18. doi:10.1186/s12876-014-0189-7
- Singh V, Haupt M, Geller D, Hall J, Diez P. Less common etiologies of exocrine pancreatic insufficiency. World J Gastroenterol. 2017;23(39):7059-7076. doi:10.3748/wjg.v23.i39.7059
- Bianconi E, Piovesan A, Facchin F et al. An estimation of the number of cells in the human body. Ann Hum Biol. 2013;40(6):463-471. doi:10.3109/03014460.2013.807878
- Morowitz MJ, Carlisle EM, Alverdy JC. Contributions of intestinal bacteria to nutrition and metabolism in the critically ill. Surg Clin North Am. 2011;91(4):771-85, viii
- Quigley EMM. Gut bacteria in health and disease. Gastroenterol Hepatol (N Y). 2013;9(9):560-9.
- Shreiner AB, Kao JY, Young VB. The gut microbiome in health and in disease. Curr Opin Gastroenterol. 2015;31(1):69–75. doi:10.1097/MOG.0000000000000139
- Valdes AM, Walter J, Segal E, Spector TD. Role of the gut microbiota in nutrition and health. BMJ. 2018;361:k2179. Published 2018 Jun 13. doi:10.1136/bmj.k2179
- Foster J, Rinaman L, Cryan J. Stress & the gut-brain axis: Regulation by the microbiome. Neurobiol Stress. 2017;7. doi:10.1016/j.ynstr.2017.03.001
- Seaward B. Managing Stress: Principles And Strategies For Health And Well-Being. 8th ed. Burlington, MA: Jones and Bartlett; 2014.
- Blajszczak C, Bonini MG. Mitochondria targeting by environmental stressors: Implications for redox cellular signaling. Toxicology. 2017;391:84–89. doi:10.1016/j.tox.2017.07.013
- Meyer JN, Hartman JH, Mello DF. Mitochondrial Toxicity. Toxicol Sci. 2018;162(1):15–23. doi:10.1093/toxsci/kfy008
- Picard M, Wallace DC, Burelle Y. The rise of mitochondria in medicine. Mitochondrion. 2016;30:105–116. doi:10.1016/j.mito.2016.07.003
- Nunnari J, Suomalainen A. Mitochondria: in sickness and in health. Cell. 2012;148(6):1145–1159. doi:10.1016/j.cell.2012.02.035
- Julio-Pieper M, Bravo J, Aliaga E, Gotteland M. Review article: intestinal barrier dysfunction and central nervous system disorders – a controversial association. Aliment Pharmacol Ther. 2014;40(10):1187-1201. doi:10.1111/apt.12950
- Mayer E, Tillisch K, Gupta A. Gut/brain axis and the microbiota. Journal of Clinical Investigation. 2015;125(3):926-938. doi:10.1172/jci76304
- Nair AT, Ramachandran V, Joghee NM, Antony S, Ramalingam G. Gut Microbiota Dysfunction as Reliable Non-invasive Early Diagnostic Biomarkers in the Pathophysiology of Parkinson’s Disease: A Critical Review. J Neurogastroenterol Motil. 2018;24(1):30-42.
- Mirjana R. Function of the microbiota. Best Pract Res Clin Gastroenterol. 2013;27(1):5-16. doi:10.1016/j.bpg.2013.03.006
- Woodhead JL, Yang K, Oldach D, et al. Analyzing the Mechanisms Behind Macrolide Antibiotic-Induced Liver Injury Using Quantitative Systems Toxicology Modeling. Pharm Res. 2019;36(3):48. Published 2019 Feb 7. doi:10.1007/s11095-019-2582-y
- Alempijevic T, Zec S, Milosavljevic T. Drug-induced liver injury: Do we know everything?. World J Hepatol. 2017;9(10):491–502. doi:10.4254/wjh.v9.i10.491
- García-Niño W, Pedraza-Chaverrí J. Protective effect of curcumin against heavy metals-induced liver damage. Food and Chemical Toxicology. 2014;69:182-201. doi:10.1016/j.fct.2014.04.016
- Gu X, Manautou JE. Molecular mechanisms underlying chemical liver injury. Expert Rev Mol Med. 2012;14:e4. Published 2012 Feb 3. doi:10.1017/S1462399411002110
- Theel E, Pritt B. Parasites. Microbiol Spectr. 2016;4(4). doi:10.1128/microbiolspec.dmih2-0013-2015

