Join our mailing list to receive the latest health tips and updates.
You have Successfully Subscribed!
Tips to Promote Gut Health for a Healthy Body & Mind

“All diseases begin in the gut” ~Hippocrates
Hippocrates, a Greek physician who lived more than 2000 years ago and widely regarded as the father of modern medicine, believed that all diseases begin in the gut.
It is interesting to note that such claim has increasingly been supported by modern scientific research.
Indeed, the health of our gut not only affects the digestion and absorption of nutrients, but also have many far-reaching repercussions on the overall health of our body and mind.
The gut or gastrointestinal (GI) tract runs from the mouth, to the pharynx, the esophagus, the stomach, the small intestine, the large intestine, and the anus.
Gut health also includes the health and balance of gut flora (more technically called gut microbiota).
Scientific research has increasingly recognized the critical roles gut and gut microbiota play in the healthy functioning of the rest of the body including immune health, brain health, metabolic health, hormonal balance, liver & detox health, skin health, etc.
Dysfunction of the gut/gut microbiota has been associated with many chronic diseases, including GI issues (e.g., IBS, IBD, etc.), heart disease, hypertension, type-2 diabetes, obesity, food allergies/sensitivities, autoimmune diseases (e.g., rheumatoid arthritis, celiac disease, multiple sclerosis, etc.), hormonal imbalance, certain cancer, neurological/neurodegenerative diseases (e.g., Alzheimer’s/dementia, Parkinson’s, autism, etc.), mental disorders, chronic liver diseases, skin issues, sleep disorders, etc.
These are discussed in detail in the next section Importance of Gut Health to Our Overall Health.
For strategies to support gut health, please go to the section below Tips to Promote Healthy Gut and Gut Microbiota.
You can also learn more about how Functional Health Coaching may support you in addressing gut dysfunction and rebuilding the health of your gut here.
Importance of Gut Health to Our Overall Health
Here is a summary of how gut health affect the health of the body and mind.
- Immune health: The immune tissue in the internal lining of the gut constitutes about 70% of the entire immune system of the body.1 A healthy gut and gut microbiota is critical for a healthy immune system. Gut dysfunction and gut microbiota imbalance (or dysbiosis) can impair immune defense, promote systemic inflammation in other parts of the body, and contribute to autoimmune disorders (e.g. rheumatoid arthritis, celiac disease, multiple sclerosis, etc.) and food sensitivities/allergies (which can manifest into chronic pain, chronic fatigue, skin issues, etc.).1–8
- Brain and nervous system health: Scientific studies have increasingly recognized the interrelationship between the gut/gut microbiota and the brain, called the microbiota-gut-brain axis. The gut is often considered the second brain. Gut and gut microbiota health affects brain, neurological and mental health.9–12
- Metabolic health: Gut dysfunction and dysbiosis contribute to chronic systemic inflammation and metabolic disorders and diseases including obesity, hypertension, heart disease, type 2 diabetes, high LDL (bad) cholesterol and low HDL (good) cholesterol, etc.13,14
- Liver and detox health: Liver is the major detox organ in the body. Scientific studies have shown the inter-relationship and inter-dependency of gut and liver health. The term gut-liver axis has been introduced. Gut dysfunction and dysbiosis can contribute to and form a vicious cycle with chronic liver disease and cholestasis (impaired bile formation and bile flow).15,16
- Hormonal balance: Certain gut bacteria produces enzymes that metabolize estrogen. Accordingly, gut microbiota is a major regulator of circulating estrogen levels. Conversely, estrogen influences gut microbiota composition.23 Dysbiosis (imbalance gut microbiota) can lead to estrogen excess (dominance) or estrogen deficiency.22 Estrogen dominance can contribute to various diseases including endometriosis, uterine fibroid, polycystic ovarian syndrome (PCOS), female reproductive cancers (e.g., ovarian cancer, breast cancer), PMS, etc. Estrogen deficiency can contribute to obesity, heart disease, type 2 diabetes, osteoporosis, cognitive decline, etc.22
- Skin health: Studies have found tight coupling between gut (including gut microbiota) health and skin health. Disorders/diseases of the gut can contribute to disorders/diseases on the skin, and vice versa. The term gut-skin axis has been coined by researchers. For examples, inflammatory bowel disease and Celiac disease can manifest into psoriasis on the skin, while rosacea on the skin may be linked to pylori infection or intestinal bacterial overgrowth in the gut.20,21
- Cancer risk: Dysbiosis is associated with increased risk of colorectal cancer and esophageal cancer. 24 H. pylori proliferation and dysbiosis of gastric microbiota in the stomach is the strongest risk factor for gastric cancer.25,26 Also, as discussed above, dysbiosis can lead to estrogen dominance which in turn can increase the risk of certain cancer.
- Sleep: Gut lining produces 400 times more melatonin (the sleep hormone) than pineal gland in the brain. Gut dysfunction and dysbiosis can contribute to sleep issues such as reduced poor sleep quality and difficulty falling or staying asleep.17–19
Adverse Health Effects Associated with Gut/Gut Microbiota Dysfunction
Gut/gut microbiota dysfunction can contribute to many chronic diseases as shown in Figure 1 below.
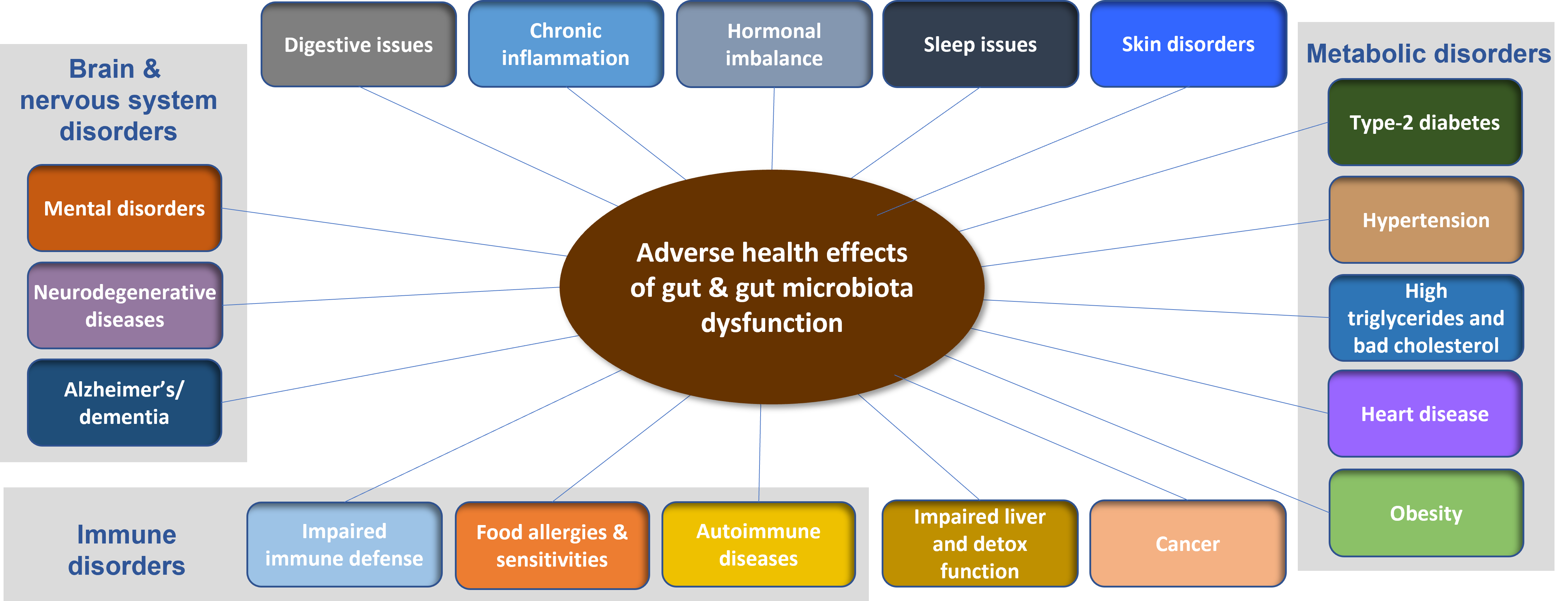
Figure 1. Adverse health effects associated with gut/gut microbiota dysfunction
Some Common Dysfunction and Disorders of the Gut
Here is a list of some common dysfunction and disorders of the gut:
- Digestive intolerance leading to GI discomforts (e.g., bloating, flatulence, belching, diarrhea, loose bowel, constipation, indigestion, etc.)
- Low stomach acid and/or insufficient digestive enzymes leading to maldigestion and malabsorption
- Acid reflux (also called gastroesophageal reflux disease or GERD)
- Gastric ulcers
- Damage/degeneration of intestinal lining including leaky gut (also called intestinal permeability)
- Imbalanced gut microbiota or dysbiosis
- Irritable bowel syndrome (IBS)
- Irritable bowel disease (IBD), including ulcerative colitis, Crohn’s disease
- Diverticulitis
- Infections in the gut (including viruses, bacteria, parasites)
For a more in-depth look at gut and digestive health and what factors contribute to gut dysfunction, please check out my previous articles: “Why Your Gut Feeling Matters”, and “You are What You Eat? Not Quite”.
In the next section, I share evidence-based tips to promote the health of our gut.
Tips to Promote Healthy Gut and Gut Microbiota
Our diet and lifestyle choices affect the health of our gut and gut microbiota. Below are some beneficial dietary and lifestyle strategies to promote the health the reduce the damage to the gut and gut microbiota.
Dietary strategies:
- Consume a whole food plant-rich diet that is high in fibers and prebiotics that feed the good gut microorganisms. (See my previous article “Simple Guideline for Healthy Eating”.)
- Avoid or minimize consumption of processed foods, artificial sweeteners, added sugars, high fructose corn syrup, and refined carbohydrates.
- Minimize exposure to toxins in foods including pesticides, herbicides, heavy metals, food additives/chemicals and other environmental pollutants. Choose organic whole foods whenever possible.
- Avoid foods that trigger immune reactions and inflammation, i.e. food allergies and sensitivities. Food allergies and sensitivities can be highly individualized and should be investigated.
- Consume probiotic-rich foods from a variety of fermented foods and/or probiotic supplement.
- Reduce consumption of foods high in saturated fats.
- Reduce or minimize alcohol consumption.
- Choose organic, grass-fed/pasture-raised meat that is free of antibiotics.
- Ensure adequate vitamin D level in the body (i.e. serum 25(OH)D levels ≥ 50 nmol/L) through sunshine and/or vitamin D supplementation.
- Ensure adequate magnesium levels in the body since magnesium plays important roles in the conversion of vitamin D to bioactive form usable by cells/tissues. (See my previous article “Hidden Magnesium Deficiency May be A Culprit to Your Health Challenges“ for tips to support healthy magnesium levels through healthy diet and lifestyle choices.)
- Be aware that certain drugs that can damage gut lining and gut microbiota including antibiotics, NSAIDs, proton pump inhibitors (PPIs), and osmotic laxatives.
Lifestyle strategies:
- Adopt adequate stress management strategies by addressing the sources of stress (e.g. through lifestyle adjustment) and practice relaxation techniques (e.g. yoga, Tai Chi, meditation, low-intensity exercise, music therapy, etc.)
- Ensure adequate sleep by practicing good sleep habits and addressing sleep issues. (See my previous article “Tips for Better Sleep to Support Your Immune Health and Overall Health”.)
Additional strategies:
- Support liver health due to tight inter-dependency between gut and liver health. (See my previous article “Take Care of Your Liver for Healthy Immunity and Overall Wellness”.)
- Address hidden gut dysfunctions which can often go undiagnosed or unrecognized, including gut infections, leaky gut, and gut inflammation. Some deep-dive investigation such as functional lab testing may be necessary (see more details in Functional Health Coaching).
- Address food sensitivities which can often be hidden. Some deep-dive investigation such as functional lab testing may be necessary (see more details in Functional Health Coaching).
Related Articles
Simple Guidelines for Healthy Eating
You are What You Eat? Not Quite
Tips for Better Sleep to Support Your Immune Health and Overall Health
Take Care of Your Liver for Healthy Immunity and Overall Wellness
Hidden Magnesium Deficiency May be A Culprit to Your Health Challenges
How to Support Your Immune Health – See What Scientific Research Showed
References
-
- Vighi G, Marcucci F, Sensi L, Di Cara G, Frati F. Allergy and the gastrointestinal system. Clin Exp Immunol. 2008;153 Suppl 1(Suppl 1):3-6.
- Quinton LJ, Walkey AJ, Mizgerd JP. Integrative Physiology of Pneumonia. Physiol Rev. 2018 Jul 1;98(3):1417-1464. doi: 10.1152/physrev.00032
- Morowitz MJ, Carlisle EM, Alverdy JC. Contributions of intestinal bacteria to nutrition and metabolism in the critically ill. Surg Clin North Am. 2011;91(4):771-85, viii.
- Quigley EMM. Gut bacteria in health and disease. Gastroenterol Hepatol (N Y). 2013;9(9):560-9.
- Mu Q, Kirby J, Reilly CM, Luo XM. Leaky Gut As a Danger Signal for Autoimmune Diseases. Front Immunol. 2017;8:598. Published 2017 May 23. doi:10.3389/fimmu.2017.00598
- Hollon J, Puppa EL, Greenwald B, Goldberg E, Guerrerio A, Fasano A. Effect of gliadin on permeability of intestinal biopsy explants from celiac disease patients and patients with non-celiac gluten sensitivity. Nutrients. 2015;7(3):1565-76. Published 2015 Feb 27. doi:10.3390/nu7031565
- König J, Wells J, Cani PD, et al. Human Intestinal Barrier Function in Health and Disease. Clin Transl Gastroenterol. 2016;7(10):e196. Published 2016 Oct 20. doi:10.1038/ctg.2016.54
- Bischoff SC, Barbara G, Buurman W, et al. Intestinal permeability–a new target for disease prevention and therapy. BMC Gastroenterol. 2014;14:189. Published 2014 Nov 18. doi:10.1186/s12876-014-0189-7
- Foster J, Rinaman L, Cryan J. Stress & the gut-brain axis: Regulation by the microbiome. Neurobiol Stress. 2017;7. doi:10.1016/j.ynstr.2017.03.001
- Julio-Pieper M, Bravo J, Aliaga E, Gotteland M. Review article: intestinal barrier dysfunction and central nervous system disorders – a controversial association. Aliment Pharmacol Ther. 2014;40(10):1187-1201. doi:10.1111/apt.12950
- Mayer E, Tillisch K, Gupta A. Gut/brain axis and the microbiota. Journal of Clinical Investigation. 2015;125(3):926-938. doi:10.1172/jci76304
- Nair AT, Ramachandran V, Joghee NM, Antony S, Ramalingam G. Gut Microbiota Dysfunction as Reliable Non-invasive Early Diagnostic Biomarkers in the Pathophysiology of Parkinson’s Disease: A Critical Review. J Neurogastroenterol Motil. 2018;24(1):30-42.
- Dabke K, Hendrick G, Devkota S. The gut microbiome and metabolic syndrome. J Clin Invest. 2019;129(10):4050-4057. doi:10.1172/JCI129194
- Teixeira TF, Souza NC, Chiarello PG, et al. Intestinal permeability parameters in obese patients are correlated with metabolic syndrome risk factors. Clin Nutr. 2012;31(5):735-740. doi:10.1016/j.clnu.2012.02.009
- Albhaisi SAM, Bajaj JS, Sanyal AJ. Role of gut microbiota in liver disease. Am J Physiol Gastrointest Liver Physiol. 2020;318(1):G84-G98. doi:10.1152/ajpgi.00118.2019
- LaRusso NF, Tabibian JH, O’Hara SP. Role of the Intestinal Microbiome in Cholestatic Liver Disease. Dig Dis. 2017;35(3):166-168. doi:10.1159/000450906
- Chen CQ, Fichna J, Bashashati M, Li YY, Storr M. Distribution, function and physiological role of melatonin in the lower gut. World J Gastroenterol. 2011;17(34):3888-98.
- Claustrat B, Leston J. Melatonin: Physiological effects in humans. Neurochirurgie. 2015;61(2-3):77-84. doi:10.1016/j.neuchi.2015.03.002
- Smith RP, Easson C, Lyle SM, et al. Gut microbiome diversity is associated with sleep physiology in humans. PLoS One. 2019;14(10):e0222394. Published 2019 Oct 7. doi:10.1371/journal.pone.0222394
- O’Neill CA, Monteleone G, McLaughlin JT, Paus R. The gut-skin axis in health and disease: A paradigm with therapeutic implications. Bioessays. 2016;38(11):1167-1176. doi:10.1002/bies.201600008
- Polkowska-Pruszyńska B, Gerkowicz A, Krasowska D. The gut microbiome alterations in allergic and inflammatory skin diseases – an update. J Eur Acad Dermatol Venereol. 2020;34(3):455-464. doi:10.1111/jdv.15951
- Baker JM, Al-Nakkash L, Herbst-Kralovetz MM. Estrogen-gut microbiome axis: Physiological and clinical implications. Maturitas. 2017;103:45-53. doi:10.1016/j.maturitas.2017.06.025
- Fernández MF, Reina-Pérez I, Astorga JM, Rodríguez-Carrillo A, Plaza-Díaz J, Fontana L. Breast Cancer and Its Relationship with the Microbiota. Int J Environ Res Public Health. 2018;15(8):1747. Published 2018 Aug 14. doi:10.3390/ijerph15081747
- Rajagopala SV, Vashee S, Oldfield LM, et al. The Human Microbiome and Cancer. Cancer Prev Res (Phila). 2017;10(4):226-234. doi:10.1158/1940-6207.CAPR-16-0249
- Wroblewski LE, Peek RM Jr. Helicobacter pylori, Cancer, and the Gastric Microbiota. Adv Exp Med Biol. 2016;908:393-408. doi:10.1007/978-3-319-41388-4_19
- Alarcón T, Llorca L, Perez-Perez G. Impact of the Microbiota and Gastric Disease Development by Helicobacter pylori. Curr Top Microbiol Immunol. 2017;400:253-275. doi:10.1007/978-3-319-50520-6_11
