Join our mailing list to receive the latest health tips and updates.
You have Successfully Subscribed!
Hidden Magnesium Deficiency May be A Culprit to Your Health Challenges

Magnesium is a critical and the 4th most abundant mineral in our body and involves in ~80% of known metabolic functions.1
However, it is estimated that 45% of US population are magnesium deficient due to diet, lifestyle, and certain health conditions.1
Yet many people could be unknowingly deficient in magnesium since chronic magnesium deficiency can often be under-recognized and underdiagnosed.2
Chronic magnesium deficiency increases the risks of a wide range of health conditions including heart disease, hypertension, type 2 diabetes, osteoporosis, muscle weakness/fatigue/cramps, mood issues (incl. irritability, depression, anxiety), sleep issues, colorectal cancer, asthma, etc.2,3,6–8
Therefore, it is important to support healthy magnesium levels in our body through adequate diet and lifestyle.
In this article, I share evidence-based information on possible causes of chronic magnesium deficiency and tips to support healthy magnesium levels.
For a quick summary of the tips to support a healthy magnesium levels, you can go directly to the Summary section.
Topic List
Overview of Functions of Magnesium
Why Chronic Magnesium Deficiency is Underdiagnosed?
Difficulty in Measuring Magnesium Status in the Body
Non-specific Signs and Symptoms in Chronic Magnesium Deficiency
Health Conditions Associated with Chronic Magnesium Deficiency
Risk Factors Contributing to Chronic Magnesium Deficiency
Foods That Drive Loss of Magnesium
Other Factors That Reduce Magnesium Absorption and Increase Magnesium Loss
Age-related Decline in Magnesium
Tips to Support Healthy Magnesium Levels
Adopt a Whole Food Plant-Rich Diet That is Rich in Magnesium
Avoid or Minimize Foods That Promote Loss of Magnesium
Adopt Stress Management Strategies
Be Aware of Factors That Affect Magnesium Status in the Body
Summary
Although chronic magnesium deficiency is quite prevalent in our society, it is often under-recognized and underdiagnosed. The reasons are explained in section Why Chronic Magnesium Deficiency is Underdiagnosed?.
Chronic magnesium deficiency cannot be overlooked as it can affect many aspects of our health and increase the risks of many chronic diseases, as described in section Health Conditions Associated with Chronic Magnesium Deficiency.
There are many risk factors that contribute to chronic magnesium deficiency, ranging from diet, lifestyle and certain health conditions, as described in section Risk Factors Contributing to Chronic Magnesium Deficiency.
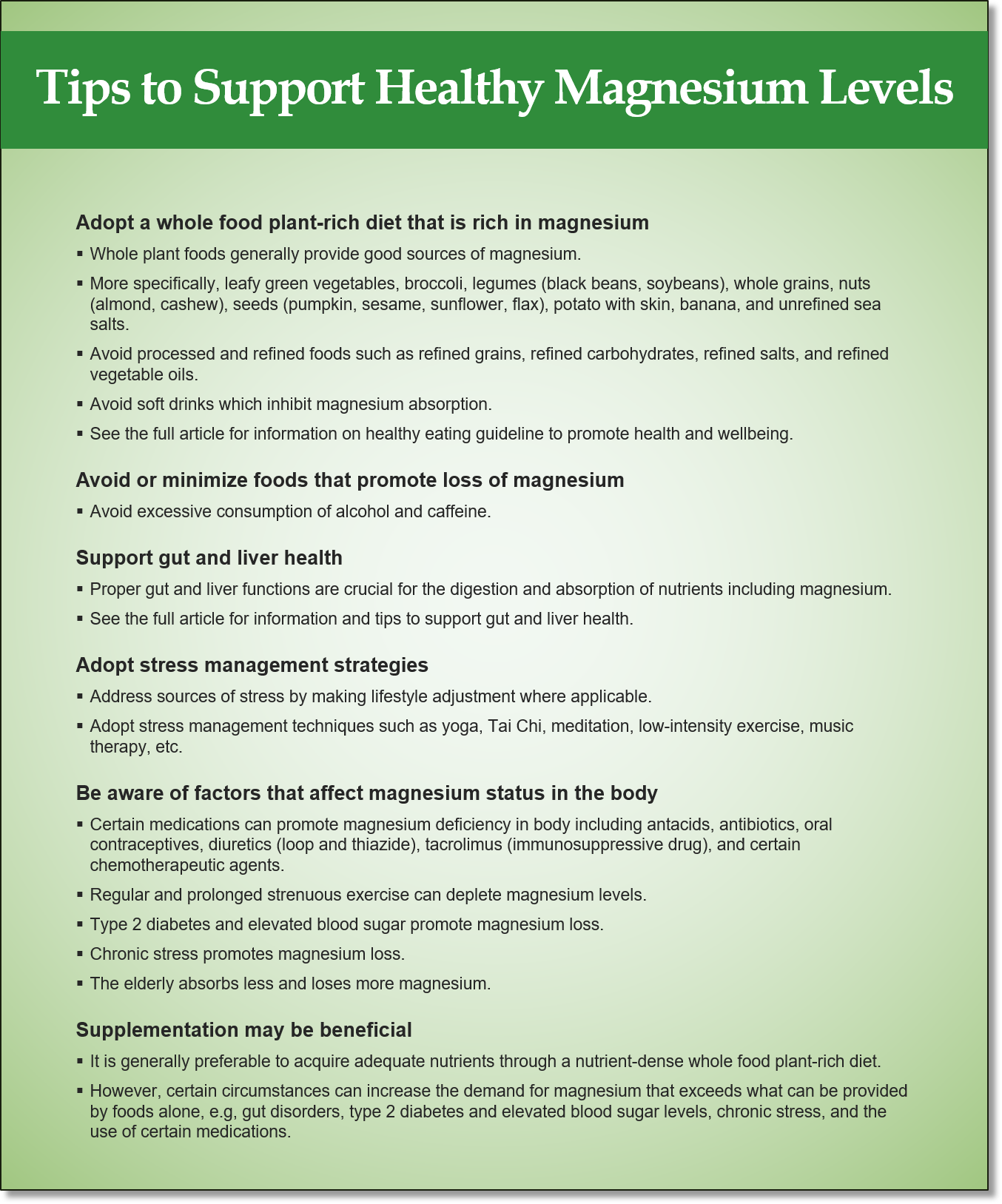
A summary of tips to support healthy magnesium levels through adequate diet and lifestyle choices, and addressing hidden health issues is given below (for more details, see section Tips to Support Healthy Magnesium Levels).
Overview of Functions of Magnesium
Magnesium is essential for maintaining normal cellular and organ functions. Some of the important functions of magnesium are listed below:1,3,4
- Serves as a cofactor or activator in more than 600 enzymes in the body.
- Contributes to structural development of bones.
- Required for the synthesis of genetic materials (i.e., DNA, RNA).
- Supports energy metabolism.
- Regulates blood glucose and blood pressure.
- Support muscle and nerve functions, and normal heart rhythm.
- Supports antioxidant level maintenance in the cell.
- Supports the conversion of vitamin D to bioactive form that is usable by cells and tissues. Note that vitamin D from sunshine or from dietary supplement needs to be converted to bioactive form in the liver and kidneys before it is usable by cells/tissues. Magnesium plays a key role in this conversion process.
Because of its wide-ranging functions, deficiency in magnesium can contribute to many health conditions as described in below.
Why Chronic Magnesium Deficiency is Underdiagnosed?
Although chronic magnesium deficiency is prevalent as described above, it is often underdiagnosed and under-recognized due to the challenges described below.
Difficulty in Measuring Magnesium Status in the Body
It is difficult to measure magnesium status in the body because magnesium is distributed mostly in the bone (~60%) and inside cells (~40%). Only less than 1% of magnesium is in blood serum.2
Magnesium level in blood serum does not reflect magnesium status within cells and bone. Regular blood test therefore is not an adequate assessment method.2,4
Other measurement methods include 24-hour urinary content, red blood cell (RBC) magnesium content, magnesium loading test, and hair magnesium content; some of which are costly, complex and not widely used.1
Hair mineral analysis test may be a cost-effective method to assess the status of magnesium and other minerals in the body and can also reveal heavy metal toxicity (e.g. mercury, lead, arsenic, etc.) in the body.1
For more information on the use of hair mineral analysis test to assess magnesium status, hidden stressors and healing opportunities in the body, please check out Functional Health Coaching here.
Non-specific Signs and Symptoms in Chronic Magnesium Deficiency
Magnesium deficiency can manifest into either acute hypomagnesaemia or chronic magnesium deficiency.
Acute hypomagnesaemia occurs when blood serum magnesium level drops below the normal range of 0.75 – 0.95 mmol/L.4
Acute hypomagnesaemia produces overt symptoms wherein milder symptoms include loss of appetite, nausea, vomiting, fatigue and weakness; and more severe symptoms include numbness, tingling, cramps, seizures, personality changes, abnormal heart rhythms and coronary spasms.4
Therefore, acute hypomagnesaemia can be diagnosed more straightforwardly through blood test and clinical sign/symptom assessment.4
Because the kidneys tightly control magnesium level in the blood through regulating urinary excretion of magnesium, acute hypomagnesaemia is uncommon among healthy people despite low dietary intake of magnesium.4
However, acute hypomagnesaemia can occur among people with certain health conditions, chronic alcoholism, and/or the use of certain medications that lead to poor absorption in the gut and excessive losses through urine.4
Acute hypomagnesaemia requires urgent attention through oral or intravenous magnesium replacement therapy.5
Chronic magnesium deficiency, on the other hand, does not show up in regular blood test as serum magnesium level is still tightly controlled by the kidneys to be within the normal range despite low magnesium in cells and bone.2,3
Unlike acute hypomagnesaemia, chronic magnesium deficiency does not have specific and unique signs and symptoms that can pinpoint to a diagnosis.2,3
Therefore, chronic magnesium deficiency can often be under-recognized and under-diagnosed among the population.2,3
Note that chronic magnesium deficiency may eventually progress into acute hypomagnesaemia when the normal serum magnesium level can no longer be maintained.2
Health Conditions Associated with Chronic Magnesium Deficiency
Although chronic magnesium deficiency may not present acute and overt signs and symptoms, it is an underlying or hidden stressor that can contribute to a wide range of health conditions.
Some of these health conditions include:2,3,6–8
- Cardiovascular disease (CVD), including abnormal heart rhythm, abnormal vascular tone, coronary heart disease, congestive heart failure, and hypertension.
- Metabolic syndrome, a cluster of conditions that include hypertension, elevated blood glucose level, excess abdominal fat, high triglyceride level, and low HDL (or good) cholesterol.
- Type 2 diabetes and impaired glucose tolerance.
- Loss of bone mass, osteoporosis and osteopenia.
- Muscular disorders, including muscle weakness, fatigue, numbness, tingling, spasms/cramps/tetany and fibromyalgia.
- Neurological disorders including mood issues (irritability, depression, anxiety), migraines and stroke.
- Colorectal cancer.
- Asthma.
- Poor sleep quality and insomnia.
- Impaired synthesis of bioactive form of vitamin D, which in turn affects bone health and impairs immune function. Magnesium deficiency can lead to vitamin D deficiency and related health conditions. (For more information on vitamin D and immune health, please check out my article How to Support Your Immune Health – See What Scientific Research Showed.)
- Chronic low-grade inflammation and oxidative stress, which are major culprits of many chronic diseases including metabolic syndrome, diabetes, heart disease, Alzheimer’s disease, cancer, etc. (For more information on how diet and lifestyle may drive or mitigate chronic inflammation/oxidative stress and chronic diseases, please check out my article How to Support Your Immune Health – See What Scientific Research Showed.)
Risk Factors Contributing to Chronic Magnesium Deficiency
By understanding the risk factors that contribute to chronic magnesium deficiency, we can adopt adequate diet and lifestyle that mitigate such risk factors.
Risk factors that contribute to chronic magnesium deficiency are described below.
Low Dietary Intake
Dietary choice is a major risk factor to low magnesium intake.
In the US, the Recommended Dietary Allowances (RDAs) of magnesium by the Institute of Medicine (IOM) is 400 – 420 mg/day and 310 – 320 mg/day respectively for adult males and non-pregnant, non-lactating adult females.4
It is estimated that 60% of people do not meet their RDA of daily magnesium intake.1
Whole plant foods are good sources of magnesium. These include leafy green vegetables, broccoli, legumes (black beans, soybeans), whole grains, nuts (almond, cashew), seeds (pumpkin, sesame, sunflower, flax), potato with skin, banana, and unrefined sea salts.2–4,9
In general, foods that are high in fiber provide magnesium.4
Food processing and refining such as refined grains, refined carbohydrates, refined salts, and refined vegetable oils, can cause a loss of up to 80% of magnesium content.1
Therefore, a diet that is low in the above whole plant foods and high in processed and refined foods is the major reason for low magnesium intake.1,2–4,9
Certain cooking methods such as boiling vegetables can lead to loss of 80% to 90% of magnesium content.9
In addition, consumption of soft drinks, which contain high phosphoric acid, can inhibit magnesium absorption in the gut.9
Drinking water can also be a source of magnesium. Hard water is rich in magnesium, whereas soft water and purified water are low in magnesium.2,9
Depletion of Minerals in Soil
There is a steady decline in magnesium and other mineral content in cultivated fruits and vegetables, attributed to depletion of these minerals in soil over the past 100 years.1
Modern farming techniques such as selective breeding, mono-cropping and the use the phosphate-based fertilizers have resulted in mineral depletion in soil.1,9
Magnesium levels have dropped by 80-90% in the US.1
Foods That Drive Loss of Magnesium
Magnesium homeostasis (or balance) in the body is tightly controlled by the kidneys.1–3
The kidneys regulate reabsorption and excretion of magnesium in the urine.1–3
Excessive loss of magnesium through urine is a common cause of low magnesium stores in the body.1–3
Certain foods have diuretic effects and promote urinary magnesium loss. Such foods include alcohol and caffeine.1–3
Poor Digestion and Absorption
Gut (or gastrointestinal) disorders that impair digestion and absorption can result in malabsorption of magnesium from foods we ingest.2,9,11
Some of the gut disorders that affect digestion and absorption include Crohn’s disease, Celiac disease, digestive enzyme deficiency, low bile secretion (due to liver and gallbladder dysfunction), low stomach acid, gut infections, etc.2,4,9,11
For more information on gut health, please check out my previous articles: Why Your Gut Feeling Matters, You are What You Eat? Not Quite.
For more information on liver health, please check out my previous article: Take Care of Your Liver for Healthy Immunity and Overall Wellness.
Other Factors That Reduce Magnesium Absorption and Increase Magnesium Loss
Certain common medications can impair magnesium absorption in the gut, including antacids, antibiotics, and oral contraceptives.1,3
Certain medications including diuretics (loop and thiazide), tacrolimus (immunosuppressive drug), and certain chemotherapeutic agents can cause abnormally high magnesium excretion in the urine.1,3
Regular and prolonged strenuous exercise can deplete magnesium levels in blood plasma, due to increased loss through sweat and urine, and redistribution of magnesium to cells and tissues.2,10
Type 2 diabetes, insulin resistance and elevated blood sugar promote magnesium deficiency due to increased urinary excretion of magnesium.4
In addition, stress can also increase urinary excretion of magnesium.12
Age-related Decline in Magnesium
The elderly absorbs less and loses more magnesium.1,3
In addition, estrogen plays important roles in enhancing magnesium uptake by soft and hard tissues.1,3
Decline is estrogen levels in postmenopausal women and elderly men further contributes to magnesium deficiency.1,3
Tips to Support Healthy Magnesium Levels
Our diet and lifestyle play important roles in mitigating the above-described risk factors of chronic magnesium deficiency.
The followings are some tips to promote healthy magnesium levels in the body.
Adopt a Whole Food Plant-Rich Diet That is Rich in Magnesium
As previously discussed, whole plant foods generally provide good sources of magnesium, in particular leafy green vegetables, broccoli, legumes (black beans, soybeans), whole grains, nuts (almond, cashew), seeds (pumpkin, sesame, sunflower, flax), potato with skin, banana, and unrefined sea salts.
Processed and refined foods such as refined grains, refined carbohydrates, refined salts, and refined vegetable oils should be avoided or minimized.
Soft drinks which inhibit magnesium absorption should be avoided.
For more information on healthy eating guideline to promote health and wellbeing, please check out my previous article: Simple Guidelines for Healthy Eating, Are Carbs and Sugars All Bad.
Avoid or Minimize Foods That Promote Loss of Magnesium
Avoid excessive consumption of alcohol and caffeine which promote loss of magnesium through urine.
Support Gut and Liver Health
As previously discussed, proper gut and liver functions are crucial for the digestion and absorption of nutrients including magnesium.
For more information and tips to support gut health, please check out my previous articles: Why Your Gut Feeling Matters, You are What You Eat? Not Quite.
For more information and tips to support liver health, please check out my previous article: Take Care of Your Liver for Healthy Immunity and Overall Wellness.
Adopt Stress Management Strategies
Stress affects many aspects of our health, not just magnesium status in the body.
It is important to manage stress by addressing the sources of stress as well as adopting certain stress management techniques such as yoga, Tai Chi, meditation, low-intensity exercise, music therapy, etc.
Be Aware of Factors That Affect Magnesium Status in the Body
As previously discussed, medications that promote magnesium deficiency in the body include antacids, antibiotics, oral contraceptives, diuretics (loop and thiazide), tacrolimus (immunosuppressive drug), and certain chemotherapeutic agents.
Regular and prolonged strenuous exercise can also deplete magnesium levels.
Type 2 diabetes/elevated blood sugar and chronic stress can increase magnesium loss through urine.
The elderly absorbs less and loses more magnesium.
The above factors increase the demand for magnesium and may warrant highly dietary intake or supplementation.
What About Supplementation?
It is generally preferable to acquire adequate nutrients through a nutrient-dense whole food plant-rich diet. Such a diet can provide adequate daily supply of magnesium to the body.
However, certain circumstances can increase the demand for magnesium that exceeds what can be provided by foods alone. Such circumstances include gut disorders, type 2 diabetes and elevated blood sugar levels, chronic stress, and the use of certain medications.
Oral Magnesium Supplementation
A common unpleasant side effect of oral magnesium supplementation is bowel intolerance and diarrhea.2,3,9
There are different forms of oral magnesium supplements, some are better absorbed, better tolerated and more bioavailable than others.2,3,9
Studies have shown that organic or chelated forms such as magnesium citrate, lactate, malate, and glycinate are better absorbed, tolerated and more bioavailable.2,3,9
Inorganic or non-chelated forms such as magnesium sulfate, chloride or oxide are less readily absorbed and less tolerable.2,3,9
The adequate dosage of oral magnesium supplement is dependent on bioavailability of the form of magnesium supplement taken, health conditions, use of certain medications, diet and lifestyle.2,3,9
Bowel intolerance often acts as a limiting factor to the intake amount of oral magnesium supplement. A dosage below the IOM recommended Tolerable Upper Intake Level (UL) of 350 mg/day is generally tolerated.4,9
It may take 20 to 40 weeks of daily magnesium supplementation to restore adequate magnesium levels in cells and bone.2
Topical Magnesium Application
Topical application of magnesium, such as magnesium oil, cream and Epsom salt, can be used alone or to augment oral magnesium supplementation.3
Topical application has the benefit of avoiding the undesirable side effect, i.e., bowel intolerance, of oral supplementation.3
When applied directly to the affected area, topical application can relieve muscle strains, cramps, and skin rashes.3
Risks of Excessive Magnesium Intake
There are no reported cases of hypermagnesemia (serum magnesium level > 1.05 mmol/L) from foods alone, even in people with impaired kidney functions.2,4,9
Because kidneys eliminate excess magnesium in the urine, hypermagnesemia from magnesium supplementation is rare among people with healthy kidney function.2,4,9
Symptomatic magnesium toxicity (when serum magnesium level exceeds 1.74-2.61 mmol/L) have been reported with extremely high doses (more than 5000 mg/day) of magnesium supplement.2,4,9
Related Articles
How to Support Your Immune Health – See What Scientific Research Showed
Simple Guidelines for Healthy Eating
You are What You Eat? Not Quite
Take Care of Your Liver for Healthy Immunity and Overall Wellness
References
-
- Workinger JL, Doyle RP, Bortz J. Challenges in the Diagnosis of Magnesium Status. Nutrients. 2018;10(9):1202. Published 2018 Sep 1. doi:10.3390/nu10091202
- Ismail AAA, Ismail Y, Ismail AA. Chronic magnesium deficiency and human disease; time for reappraisal?. QJM. 2018;111(11):759-763. doi:10.1093/qjmed/hcx186
- Razzaque MS. Magnesium: Are We Consuming Enough?. Nutrients. 2018;10(12):1863. Published 2018 Dec 2. doi:10.3390/nu10121863
- National Institute of Health. Magnesium – Fact Sheet for Health Professionals. Ods.od.nih.gov. https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/. Published 2020.
- Fulop T, Agarwal M, Keri K. Hypomagnesemia. Emedicine.medscape.com. https://emedicine.medscape.com/article/2038394-overview. Published 2018.
- Uwitonze AM, Razzaque MS. Role of Magnesium in Vitamin D Activation and Function. J Am Osteopath Assoc. 2018;118(3):181-189. doi:10.7556/jaoa.2018.037
- Ji X, Grandner MA, Liu J. The relationship between micronutrient status and sleep patterns: a systematic review. Public Health Nutr. 2017;20(4):687-701. doi:10.1017/S1368980016002603
- Djokic G, Vojvodić P, Korcok D, et al. The Effects of Magnesium – Melatonin – Vit B Complex Supplementation in Treatment of Insomnia. Open Access Maced J Med Sci. 2019;7(18):3101-3105. Published 2019 Aug 30. doi:10.3889/oamjms.2019.771
- Tarleton EK. Factors influencing magnesium consumption among adults in the United States. Nutr Rev. 2018;76(7):526-538. doi:10.1093/nutrit/nuy002
- Laires MJ, Monteiro C. Exercise, magnesium and immune function. Magnes Res. 2008;21(2):92-96.
- van der Heide F. Acquired causes of intestinal malabsorption. Best Pract Res Clin Gastroenterol. 2016;30(2):213-224. doi:10.1016/j.bpg.2016.03.001
- Grases G, Pérez-Castelló JA, Sanchis P, et al. Anxiety and stress among science students. Study of calcium and magnesium alterations. Magnes Res. 2006;19(2):102-106.
